Advancement of research and translation of evidence into pediatric physical therapy practice is one of the goals of the APTA Pediatrics Strategic Plan.
To meet this goal, APTA Pediatrics carries out a number of activities to support and promote research, including research grants, research awards, research summits, and review of abstracts for conferences.
Have a question about APTA Pediatrics Research? Contact the Director of Research.
Researcher Spotlight - Kristie F Bjornson, PT, PhD, MS
 Kristie F Bjornson
PT, PhD, MS
Kristie F Bjornson
PT, PhD, MS
Kristie Bjornson, PT, PhD, MS is Professor of Developmental Medicine and Adjunct Research Professor of Rehabilitation Medicine at the University of Washington and Seattle Children’s Hospital Research Institute. Dr. Bjornson completed her physical therapy degree at the University of Minnesota and her Master’s in Rehabilitation Science and PhD in Nursing Science at the University of Washington, Seattle, WA. Dr. Bjornson’s doctoral work was the first to document community-based ambulatory activity via wearable sensors in adolescents with cerebral palsy as well as self-reported quality of life supported by a NINDS NRSA pre-doctoral fellowship.
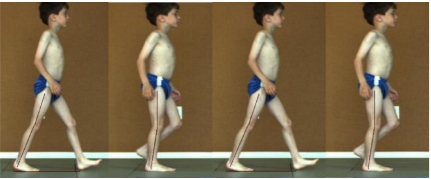
Dr. Bjornson is a pediatric physical therapist with over 40 years of clinical experience in settings such as the NICU, public schools, birth-to-three centers, and at Seattle Children’s Hospital (SCH). Dr Bjornson was the research coordinator for the Spasticity Management Clinic at SCH, serving as the project coordinator for the randomized clinical trial and meta-analysis of selective dorsal rhizotomy, botulinum toxin-A and a descriptive cross-sectional study of intrathecal baclofen (ITB) therapy. Dr. Bjornson’s doctoral work focused on the assessment of physical activity, health, and quality of life in ambulatory children with cerebral palsy (CP) and normative ambulatory data for the StepWatch accelerometer.
Dr Bjornson completed an NICHD NIH K23 career development award focusing on the measurement of ambulatory physical activity, participation in daily life of children with CP and the influence of orthotics. Her ongoing current NIH funded research includes a study of power training combining the Total Gym and treadmills, a home-based treadmill training study and a project examining the Ankle-Foot Orthoses Footwear Combination (AFO-FC) orthotic management approach for ambulatory children with CP. See Bjornson Lab Seattlechildrens.org). Dr. Bjornson also has a small private practice focusing on orthotics management across the lifespan.
Research Grants Funded by APTA Pediatrics
2025 APTA Pediatrics Research Grant Recipients (total funded: $30,000)
- Elizabeth Maus PT, DPT, PhD(c): Telehealth training to promote device-supported standing and walking in children with severe motor delays (Research Grant Sponsored by Rifton Equipment, $10,000)
- Rachel Bican, PT, DPT, PhD: Feasibility and Acceptability of an Intensive Telerehabilitation Parent-Coaching Program for Young Children with Motor Delays in Rural Appalachia (Academy Research Grant Application, $10,000)
- Beth A. Smith, PT, DPT, PhD: Exploring the role of interhemispheric coherence in hand dominance and motor development (Academy Research Grant Application, $10,000)
2024 APTA Pediatrics Research Grant Recipients (total funded: $25,000)
- Dr. Lisa Gradziel: The Impact of Adaptive Cycling on Heart Rate Response in Children and Adults with Medical Complexity (Research funded by Rifton: $10,000)
- Dr. Jessica Trenkle: Implementation of a direct NICU-to-home service delivery model for at-risk infants through the State of Illinois Early Intervention Program (Planning: $15,000)
2023 APTA Pediatrics Research Grant Recipients (total funded: $52,500)
- Dr. Tori Marchese: Sickle Cell Children’s Exercise Study (SuCCESs): Determining the effects of a targeted exercise training program on neuromuscular performance, locomotor efficiency, and exercise tolerance in children with sickle cell disease (Research 1: $30,000)
- Dr. Shaaron Brown: General Movement Optimality Score as a Biomarker in Early Detection of Neurodevelopmental Disability in Extremely Preterm Infants. (Mentored: $10,000)
- Dr. Ketaki Inamadar: A novel AI-based approach for quantitative assessment of postural control during prone play in infancy: A Proof-of-Concept Study. (Research 2: $10,000)
- Dr. Jessica Silveira: Effect of Rehabilitation Interventions that Embed Play on Motor, Cognitive, Language, and Behavioral Development in Young Children with or at Risk for Motor Delays (Systematic Review). (Critical Synthesis of Literature Grant: $2,500)
2023 APTA Pediatrics Mentored Writing Scholarship (total awarded= $500)
- Dr. Sandra Ribeiro (clinician) and Dr. Kim Wynarczuk (mentor). Case Study: Clinical decision making for two students with bilateral limb loss in the educational setting.
2022 APTA Pediatrics Research Grant Recipients (total funded = $107,219)
- Planning Grant: Adults with CP: Patient Reported outcome Registry Enrollment. PI: Mary Gannotti. Amount awarded: $28,000
- Research 1 Grant: Assessing the Impact of Exercise Based Intensive Interdisciplinary Pain Treatment (IIPT) on Endogenous Pain Modulation in Youth with Chronic Pain Syndromes. PI: Julie Shulman. Amount Awarded: $29,626.
- Research 1 Grant: Reliability and Construct Validity of the Functional Symmetry in Congenital Muscular Torticollis. PI: Mary Rahlin. Amount Awarded: $30,000.
- Mentored Grant: Identifying Early Signs of Motor Impairment in Infants with Spinal Muscular Atrophy. PI: Melissa McIntyre. Amount Awarded: $9,943.
- Mentored Grant: Associations Between Infant Motor Development and Parent-Infant Relationships. PI: Corri Stuyvenberg. Amount Awarded: $9,650.
2022 APTA Pediatrics Mentored Writing Scholarships (total awarded=$1,000)
- Jenna Lammers (clinician) and Barbara Smith (mentor). Case study: Therapeutic Play Gym: Feasibility of a caregiver-mediated exercise system for infants and young children with severe neuromuscular weakness.
- Debra Depto (clinician) and Cesar Guilherme (mentor). Case study: SDR short term-effects on reactive postural control in a child with cerebral palsy (Gross Motor Classification System II).
2021 APTA Pediatrics Research Grant Recipients (total funded = $112,103)
- Critical Synthesis of Literature Grant: Efficacy of Rehabilitation Professional-Provided Parenting Interventions for Families with Young Children with Developmental Disabilities, Ages Birth to Three Years. PI: Corri L. Stuyvenberg. Amount awarded: $2,500.
- Critical Synthesis of Literature Grant: Effect of Motor Interventions on Cognition, Communication, and Social Interaction in Children with Autism Spectrum Disorder. PI: Judy Zhou and Stacey Dusing; Amount: $2,500.
- Mentored Research Grant: Effects of Posture and Seating on Learning Opportunities in
Infants at Risk for Cerebral Palsy. PI: Kari Kretch. Amount awarded: $10,000. - Research II Grant: Interaction between Self-Propelled Mobility and Spatial Cognition in Infants and Toddlers with Spina Bifida. PI: Monica Rivera. Amount awarded: $7,355.
- Research I Grant: Up and Down: Use of a Dynamic Partial Body Weight Support Play Environment to Encourage Upright Mobility and Exploration in Infants with Down Syndrome. PI: Heather A. Feldner. Amount Awarded: $29,782.
- Research I Grant: Examining Visual Strategies in Motor Planning and Execution in Children with Hemiparetic Cerebral Palsy. PI: Rachel Hawe. Amount Awarded: $29,966.
- Research I Grant: Remote Ischemic Conditioning to Enhance Bimanual Skill Learning and Corticospinal Excitability in Children with Unilateral Cerebral Palsy. PI: Swati M. Surkar. Amount Awarded: $30,000.
- Research I Grant: Interaction between Self-Propelled Mobility and Spatial Cognition in Infants and Toddlers with Spina Bifida. PI: Monica Rivera. Amount Awarded: $7,355.
2020 APTA Pediatrics Research Grant Recipients (total funded = $117,113.18)
- Planning Grant: Development of a research consortium and planning a proposal to evaluate the efficacy of STEPS_H2 - Supporting Transitions by Enhancing Parent Support from Hospital to Home (PI: Stacey Dusing)
- Research Grant I: Effects of attentional focus on motor learning in children with autism spectrum disorder (PI: Jamie Holloway)
- Research Grant I: MicroRNAs as key regulators of gene expression in skeletal muscle of children with cerebral palsy (PI: Noelle Moreau)
- Mentored Grant: Just in TIME: The need for timely disclosure of CP diagnoses in primary care practices (PI: Madalynn Wendland)
- Mentored Grant: Measuring physical activity in non-ambulatory youth with CP, GMFCS IV-V during daily routines (PI: Nia Mensah)
- Mentored Grant: Exploring the impact of emotional availability on the efficacy of physical therapy intervention (PI: Rebecca Molinini)
- Critical Synthesis of Literature Grant: Early markers of motor delay in ASD during the first two years of life: A Systematic Review (PI: Maninderjit Kaur)
2019 APTA Pediatrics Research Grants Recipients (total funded = $86,566.77)
- RFA Planning Grant - "An individualized multimodal intervention for bone and muscle health in pre-adolescents with cerebral palsy: promoting healthy transitions into adulthood" by Susan V. Duff, MPT, OT/L, EdD, Noelle G. Moreau, PT, PhD, Kathleen M Friel, PhD;
- RFA: Research Grant - Understanding transition to community-based therapy services following Neonatal Intensive Care Unit hospitalization: physical therapy timing, dose, and functional outcomes by Beth McManus, PT, MPH, ScD;
- Mentored Research Grant - "Early Intervention for the Caregiver-Infant Dyad with Neonatal Abstinence Syndrome: A Case Series" by Kara Boynewicz, PT, DPT, ATC, Board-Certified Clinical Specialist in Pediatric Physical Therapy;
- Mentored Research Grant - "Examination of a Power Leg Press (PLP) Test in Cerebral Palsy: Reliability, Sensitivity to Change and Functional Significance" by Mattie Pontiff, PT, DPT;
- Mentored Research Grant - "Comprehensive Measurement of Intervention Fidelity" by Kimberley S. Scott, PT, DPT, Board-Certified Clinical Specialist in Pediatric Physical Therapy;
- Research Grant 2 - "Participation of students with disabilities on school trips: Parent experiences and perceptions" by Kimberly D. Wynarczuk, PT, PhD, MPH, Board-Certified Clinical Specialist in Pediatric Physical Therapy.
2018 APTA Pediatrics Research Grant Recipients (total funded = $95,852)
- Mentored grant went to Megan Flores for her study titled: An investigation of trunk control in young children with Down Syndrome
- Mentored grant to Jason Cook titled Caring for Children with Severe Cerebral Palsy: The Lived Experience of Parents.
- Mentored grant to Jeongah Kim titled Using Exploratory Learning to Encourage Selective Hip-knee Joint Movement in Infants Born Full-term and Very Preterm
- Research II grant to Alyssa Fiss titled Gaining insight and Understanding of Experiential Learning in Pediatrics PT Education.
- Research I grant to Kristin Krosschell titled Mixed Methods Study of Utilization Patterns of Modified Ride on Vehicles for Kids With Developmental Delay
- Research I grant to Barbara Sargent titled Understanding Selective Motor Control of Infants at High Risk for Cerebral Palsy

